EHR for Radiology (RIS + PACS)
Capabilities, Integrations, Costs
Since 2005 in healthcare software engineering, ScienceSoft delivers RIS-centric EHR systems specifically designed for radiology workflows. Our solutions help radiologists and technologists streamline their workflows, cut report turnaround, and reduce manual hand‑offs.
EHR for Radiology in Brief
Radiology EHR is a RIS-centric radiology platform with integrated or native PACS/VNA modules, covering end-to-end imaging workflows, from scheduling and modality worklists to charge capture and results distribution. The solution can be implemented as an additional RIS layer on top of an existing PACS and/or an enterprise electronic health/medical records system, or as a full-scale radiology management system with native picture archiving and optional VNA.
Valuable integrations for radiology EHR: imaging devices (modalities), enterprise EHR and/or HIE, PACS/VNA (if already in place), diagnostic support module, patient and referring physician portals, a teleradiology platform, and billing/RCM software or a clearinghouse.
Implementation time: 4–6 months for an RIS‑first MVP; 6–12+ months for RIS + native PACS.
Development costs: $200,000–$300,000+ for an RIS-first MVP integrated with the existing PACS and EHR; $400,000–$800,000+ for RIS + native PACS; $1,000,000–$2,000,000+ for a full-fledged radiology platform with RIS + native PACS + VNA + multi-site routing/load-balancing, analytics, and AI assistance (triage, NLP/report help), with enterprise-grade rollout. Use our free online calculator to get a custom quote from our consultants.
Why Radiology Teams Modernize Their RIS Setups
Radiology departments today face challenges that make a centralized, custom-built radiology platform increasingly appealing:
- Fragmented imaging environments. Multi-site healthcare networks often run separate RIS and PACS systems, creating delays in image access, report sharing, and care coordination. Enterprise imaging consolidation in one radiology platform with cloud PACS access can help unify processes, ease multi-site image access, and make the end-to-end radiology workflow smoother and faster.
- Growing imaging backlog. Backlogs in image reading and reporting are rising due to workforce shortages, reimbursement cuts, and the overutilization of medical imaging. AI and teleradiology capabilities embedded directly into a custom radiology platform can solve this problem by reducing the manual steps, equipping radiologists with another pair of eyes, and enabling remote consultations.
Key Features of EHR/EMR Software for Radiology
Below you will find an outline of essential and advanced software capabilities most frequently requested by ScienceSoft’s clients in radiology. We tailor each solution’s scope to the client’s specific needs and workflows.
Core features
Value-adding features
Key Integrations for a Radiology EHR
To enable automated data exchange, ScienceSoft recommends building integrations on industry standards, including HL7 v2 (dominant for orders and results), FHIR (growing for modern health data exchange), DICOM/DICOMweb (for medical imaging), and IHE XDS-I (for cross-organization image sharing). Using these as the foundation, we can help you set up the following integrations and more, depending on your IT ecosystem’s specifics: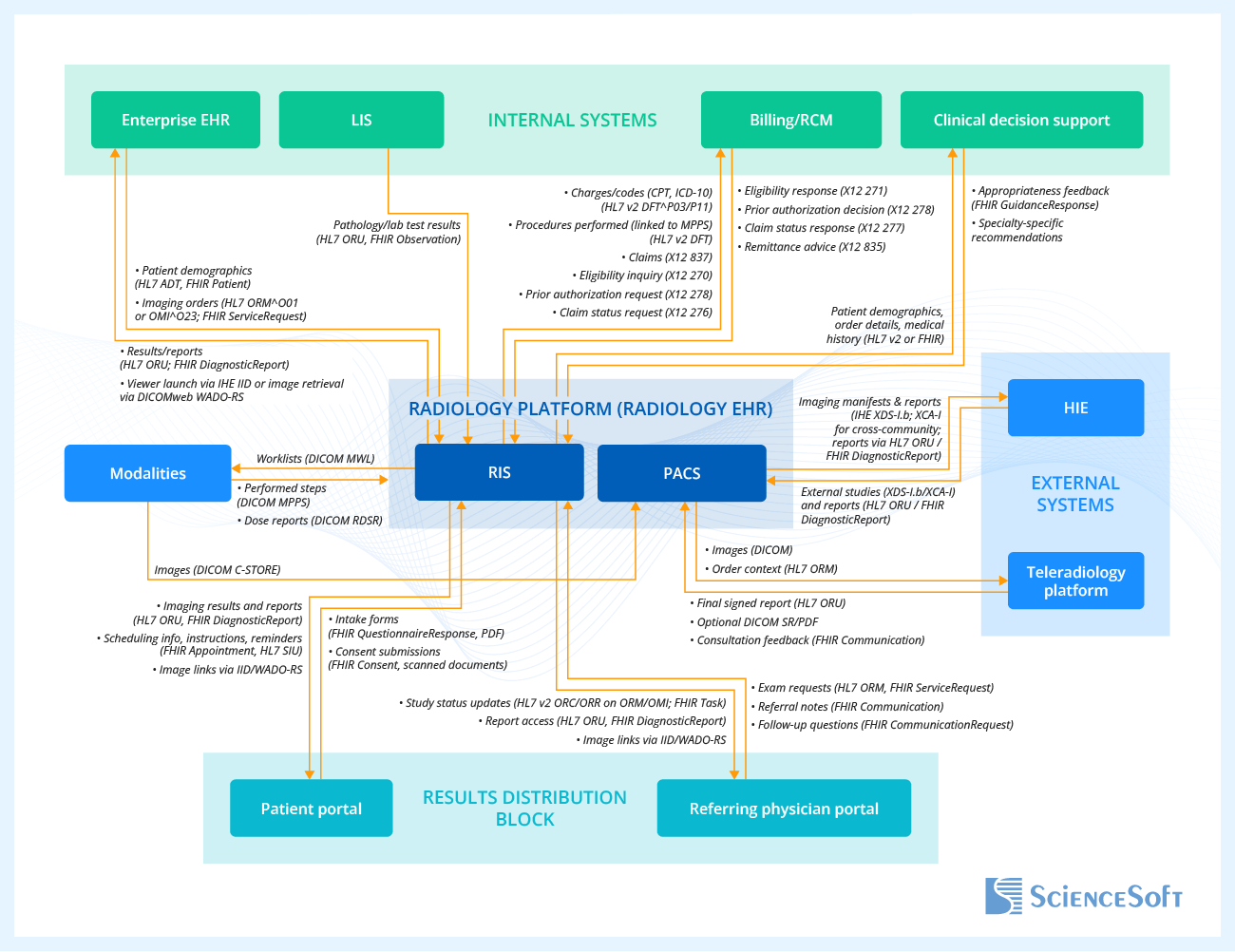 In the diagram above, ScienceSoft’s solution architects present a potential situation where the radiology EHR platform has built-in RIS and PACS modules and integrates with the enterprise EHR and billing system. In other scenarios, a radiology platform can be integrated with the organization’s existing PACS/VNA, serve as an EHR-like data store without a generic EHR, and perform revenue cycle management functions independently, via direct integration with clearinghouses. Here’s how the presented modules work:
In the diagram above, ScienceSoft’s solution architects present a potential situation where the radiology EHR platform has built-in RIS and PACS modules and integrates with the enterprise EHR and billing system. In other scenarios, a radiology platform can be integrated with the organization’s existing PACS/VNA, serve as an EHR-like data store without a generic EHR, and perform revenue cycle management functions independently, via direct integration with clearinghouses. Here’s how the presented modules work:
- Direct integration with modalities enables the system to distribute study details to modalities and receive completed studies with performed-procedure data for interpretation and reporting.
- Connection with enterprise EHR (if available) ensures real-time synchronization of patient demographics, orders, and results within the organization without the need for manual re-entry. Enterprise EHR can also serve as the central integration point for data exchange with other connected systems, including those of partnering providers. Where no general EHR is present, the radiology EHR’s RIS module can serve as the main operational hub while still supporting future integrations.
- Optional integration with the laboratory information system (LIS) allows radiologists to correlate lab results and pathology findings with imaging studies, enriching diagnostic context without leaving their reading environment.
- Integration with billing software or RCM automates eligibility checks, prior authorizations, coding, and claims. If there are no dedicated RCM tools in place, the radiology platform may interact directly with clearinghouses.
- Connectivity with a clinical decision support system (CDSS) enables embedding appropriateness criteria into imaging order workflows. It also allows support for specialty-specific workflows (e.g., a cardiac risk assessment tool for cardiology, stroke imaging protocols for neurology, lung nodule evaluation tool for pulmonology, and cancer staging support for oncology).
- An integration with a patient portal allows patients to access the imaging results and instructions, scheduling, reminders, and messaging. The portal can connect directly to the radiology platform or be integrated via enterprise EHR.
- A dedicated referring physician portal enables referring physicians to request the imaging exams, track their status, and view the images and reports. In the absence of a portal, physicians can receive results into their EHR via an HL7 interface.
- Connection to regional or national Health Information Exchanges (HIEs) enables cross-institution image and report sharing.
- Finally, integration with a teleradiology platform allows radiologists to have secure access to images and reporting tools during virtual consultations.
Key Steps of Radiology EHR Software Development
When building an EHR system tailored for radiology workflows, ScienceSoft typically takes the following key steps:
1.
Discovery and requirements engineering
We interview the main business stakeholders, like the chief of radiology, the imaging operations manager, and the referral manager, to identify their needs, expectations, and process optimization opportunities. In parallel, we define the organization’s business goals (e.g., 50% shorter turnaround times) and requirements (e.g., the system must automate result delivery to referring physicians). The findings inform the final solution vision, scope, and limitations. This information is included in the vision and scope document and is used further for project planning to define key milestones, KPIs, budget, and risk controls.
ScienceSoft’s business analysts conduct interviews with the future platform users (e.g., radiologists, technologists, admins) to identify their needs, pains, and expectations at a more granular level. This helps the discovery team clearly define user roles and their tasks to model accurate user personas and user journeys.
Simultaneously, ScienceSoft’s compliance officers define applicable regulations or certifications (e.g., HIPAA, GDPR, ONC, FDA QMSR (replacing 21 CFR Part 820), FDA 510(k), MDR, or other local regulations) and the regulatory pathways to follow. For example, if your radiology EHR platform includes a custom AI medical image analysis module that will provide diagnostic assistance, it is likely to qualify as Software as a Medical Device (SaMD). In this case, we plan for the premarket submission according to the FDA 510(k) program (US) or premarket certification by a Notified Body designated under MDR/IVDR (EU).
At the end of discovery, we create a detailed Software Requirements Specification (SRS) that will serve as the foundation for the system design and development. It covers all the functional and non-functional technical requirements for the system and serves as the foundation for system design and development.
Read more: ScienceSoft's Approach to Discovery in Software Development.
You only need ONC certification for your EHR-like platform if you participate in Medicare Promoting Interoperability (PI) or similar programs
You will likely need CEHRT if you must satisfy Medicare Promoting Interoperability requirements (e.g., for hospitals or MIPS clinicians reporting PI), or if your contract explicitly requires CEHRT. In that case, we will scope a certification path and implement the required capabilities for it. However, you likely don’t need CEHRT if you’re an independent imaging center (PI-exempt/not reporting) that needs a stand-alone, RIS-centric radiology platform, or a hospital department that relies on the hospital’s ONC-certified enterprise EHR (Epic, Cerner, etc.) for general admin workflows while your radiology platform mainly integrates and pushes imaging results into the EHR.
Either way, I recommend building any platform for HL7/FHIR interoperability to secure it for future integrations and potential regulatory changes, even if you don’t need CEHRT right now.
2.
Architecture design
Based on the findings of the discovery stage, ScienceSoft’s solution architects design a scalable and secure architecture for the solution. In the case of connected radiology platforms, we typically use a hybrid architecture: a modular monolith for the native RIS+PACS core to ensure low-latency data exchange and high reliability, surrounded with loosely coupled services for reporting, results delivery, and interoperability. This enables independent scaling and safer releases that don’t risk core uptime.
Solution architects select an optimal tech stack that can handle large imaging datasets (e.g., multi-slice CTs, mammography studies, full-body MRIs), progressive image loading (DICOMweb gateways; STOW-RS for store, QIDO-RS for query, WADO-RS for retrieve), and secure access for multiple user roles, including teleradiologists and external referring physicians.
We create detailed architectural diagrams, including component relationships, data flows, and deployment strategies. As a result, you get an architecture blueprint and integration map, plus security and resilience patterns aligned with HIPAA/GDPR.
Read more: ScienceSoft’s Approach to Software Architecture Design.
Single interface engine vs. point-to-point integrations
For this type of solution, we usually deploy an interface engine to broker orders, results, and revenue messages, which avoids riskier point-to-point links. The engine can connect the enterprise EHR ↔ RIS, RIS ↔ billing/RCM/clearinghouse, and RIS/EHR ↔ LIS/HIE/portals/teleradiology/CDS, handling HL7 v2/FHIR/X12 transformations, routing, validation, retries/queuing, and monitoring/alerts so data stays clean and issues are traceable. Where available, we can reuse the hospital’s integration engine (e.g., Infor Cloverleaf, Rhapsody/Corepoint, NextGen Connect, InterSystems IRIS for Health) to handle HL7 v2/FHIR/X12 routing, transformation, retries, and monitoring; for stand-alone imaging centers, we can add a lightweight engine to support future growth without the need to re-engineer the entire thing when the time comes.
3.
UX and UI design
ScienceSoft’s UX and UI designers create wireframes and interactive UI prototypes for all interfaces (e.g., imaging order entry, image viewing, structured and narrative reporting, and study tracking dashboards). UX specialists conduct UX testing with real radiology scenarios to validate usability across workflows (e.g., navigation through multi-series CT or MRI scans, comparing current with prior studies, and generating reports).
When creating UX and UI, we ensure the software is:
- Easy to use under pressure (e.g., in case of emergency imaging). This can be achieved via implementing large buttons, logical tab order, and simple navigation between imaging studies, patient records, and reporting tools.
- Safe by design. We implement this through pre-filled fields (e.g., based on modality type, exam type, or protocol), default options (e.g., standard protocols by body part or condition), and validation rules that align with radiology reporting logic.
- Convenient for multitasking. This can be realized via keyboard shortcuts, undo or redo features, alerts, and persistent display of important patient details (e.g., allergies, recent labs, previous imaging studies).
- Intuitive for the staff. In many cases, we can partially reuse or replicate UI elements of the software tools the team is already familiar with (e.g., generic EHR) to ease adoption and minimize friction points. This also reduces the time and budget needed for custom UI design.
As a result, you receive interactive prototypes validated with real radiology scenarios and a design consistent with your internal apps to speed adoption.
Read more: ScienceSoft’s Approach to User Convenience in Healthcare Software, How ScienceSoft Designs Software UI.
4.
Development and testing
When building healthcare software, the development process is typically less iterative than in other software engineering lines, since the scope and features are highly defined from the start and subject to less change than an average enterprise system. Instead of minor releases every 2 weeks, teams typically deliver one validated MVP and gradually evolve it with rare, larger-scale updates. The RIS+PACS core is frozen early, and any software change has to go through formal review to protect business logic integrity.
At ScienceSoft, we break development efforts into clinically meaningful increments that match software features, for example, order management + clinical decision support (appropriateness and contrast rules), and results distribution (HL7 ORU/FHIR + expiring image links to referrer EHRs and patient delivery options). Each increment has clear pass/fail criteria (e.g., ≥99.5% MWL issued, ≥95% reports delivered to referrer EHRs within 5 minutes, p95 first-image display ≤ X seconds for large CT).
As part of quality assurance, we verify DICOM/IHE behavior, HL7 v2/FHIR interfaces, and interface-engine retries/reconciliation. We also ensure radiology-specific security controls are in place: DICOM over TLS, AE-title allowlists, modality VLANs, SSO/RBAC, ATNA-style audit, and signed expiring links for images.
If you need ONC certification or if one of the software modules is considered SaMD (e.g., for diagnostic AI tools), we document the required evidence (ONC Cures, IEC 62304/14971/62366, real-world testing, proper labeling) throughout development to support regulatory submission.
As a result, you receive a deployment-ready MVP package (source code, compiled builds, deployment scripts, and configurations) as well as the documentation and validation artifacts required for production sign-off: requirements-to-tests traceability, DICOM conformance statements, interface specifications, performance baselines, security and compliance evidence, and admin/DR runbooks.
Read more: How ScienceSoft Approaches Software Development Projects.
5.
Pre-launch activities
At this stage, ScienceSoft’s experts update risk and compliance matrices. Our compliance specialists help you conduct HIPAA or GDPR audits, ONC submission, FDA pre-submission, or other submissions as required.
We also prepare user training materials, software documentation, and quick-start guides for different radiology roles. As a result, you receive a go-live readiness pack: policy and procedure updates, user guides, and quick-start playbooks.
6.
Deployment and user training
Prior study migration and DICOM tag normalization are the riskiest and most time-consuming parts. ScienceSoft’s development team starts by inventorying legacy PACS/RIS, exporting priors, and cleaning key tags (PatientID+Issuer, Accession, Study/Series/SOP UIDs, dates). We reconcile MRNs and merges, preserve or remap UIDs, re-index into the new PACS so priors open and hang correctly, and move final reports, key images, and dose (RDSR). We verify the migration with pre-/post-counts and reader spot checks.
Go-live is phased or completed during the after-hours with a ready rollback to minimize disruptions. We validate ingest, query/retrieve, the MWL/MPPS loop, and ORU/FHIR result delivery before opening the system broadly.
We also conduct role-based training of your staff in your preferred format (remote virtual sessions with screen sharing or on-site training). As performance is typically a top radiologist complaint, we closely monitor system performance (e.g., image loading speed) and radiologist feedback for 2–4 weeks post-launch. We define explicit, project-specific SLAs (e.g., p95 first-image display ≤ 2 s for a large CT on a 1 Gbps LAN; results delivery ≤ 5 min after sign-off) and validate against them during go-live.
As a result, you get a ready system with all your historical studies and images intact, a migration validation report (with before/after study counts, any fixes we made, and UID checks showing studies weren’t duplicated or lost), admin and support playbooks, and trained users.
Read more: How ScienceSoft Ensures Effective Knowledge Transfer and Training for Healthcare Software Users
How Much It Costs to Develop an EHR System for Radiology
Based on ScienceSoft’s experience, the cost of building electronic health/medical records for radiology varies significantly depending on the following factors:
- Adding a native PACS module (more expensive) vs. integration with the existing PACS.
- VNA integration (increases data storage and governance spend).
- The need for multi-site routing and load balancing.
- The volume of images that need to be migrated to the new system, and how much DICOM tag clean-up/UID reconciliation is needed.
- Viewer and speed targets (3D/tomo, complex hanging protocols, and goals like p95 first image ≤2s increase the costs).
- Results delivery requirements (many custom connections to external partners, secure/expiring image links, delivery receipts, SMART on FHIR launches increase the costs).
- In-RIS billing (more expensive) vs. integration with the existing RCM system.
- Security and resilience requirements (DICOM over TLS, SSO/RBAC, ATNA audit, strict RPO/RTO, HA/DR drills, and pentests increase the costs).
- The need to add assistive AI features, such as dictation engines.
- SaMD functionality, such as a built-in diagnostic module for image analysis.
- The need for ONC certification.
$200,000–$300,000
For an RIS-first MVP integrated with the existing PACS and enterprise EHR.
$400,000–$800,000+
For a radiology EHR platform containing RIS and native PACS modules.
$1,000,000–$2,000,000+
For a radiology platform with RIS + native PACS + VNA + multi-site routing/load-balancing, analytics, and AI assistance, with enterprise-grade rollout.
Why Choose ScienceSoft as Your Radiology Software Development Partner
- In healthcare IT since 2005.
- ISO 13485, ISO 9001, and ISO 27001 certifications.
- Experience in achieving compliance with the requirements of HIPAA, GDPR, the 21st Century Cures Act, FDA 21 CFR Part 820, FDA 510(k), MDR, IVDR, CEHRT, and 42 CFR Part 2.
- Deep knowledge of data exchange standards such as FHIR, XDS/XDS-I, C-CDA, and USCDI.
- Expertise in clinical coding and terminology standards such as ICD-10, CPT, SNOMED CT, LOINC, and RxNorm.
Our awards and partnerships
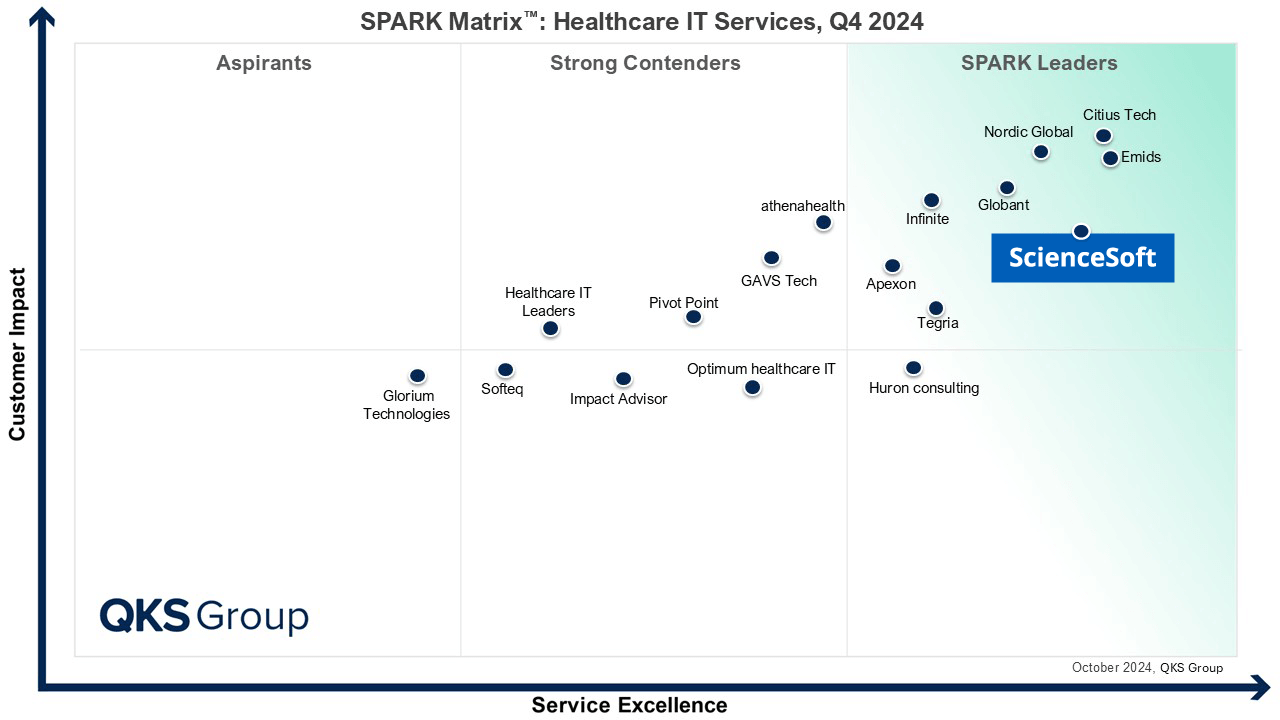
Featured among Healthcare IT Services Leaders in the 2022 and 2024 SPARK Matrix
Named among America’s Fastest-Growing Companies by Financial Times, 4 years in a row
Recognized on Newsweek’s 2025 America’s Most Reliable Companies List
Recognized by Health Tech Newspaper awards for the third time
Top Healthcare IT Developer and Advisor by Black Book™ survey 2023
Named Best in Class in Medical Device Connectivity by Frost & Sullivan (2023)
Listed in IAOP’s 2025 Global Outsourcing 100 for the 4th year running
ISO 13485-certified quality management system
ISO 27001-certified security management system






